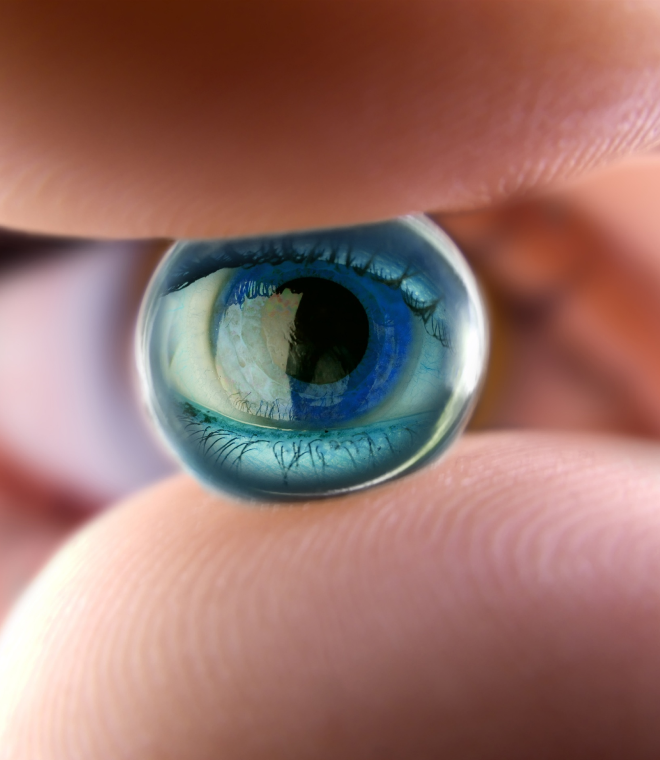
Trasplante de cornea
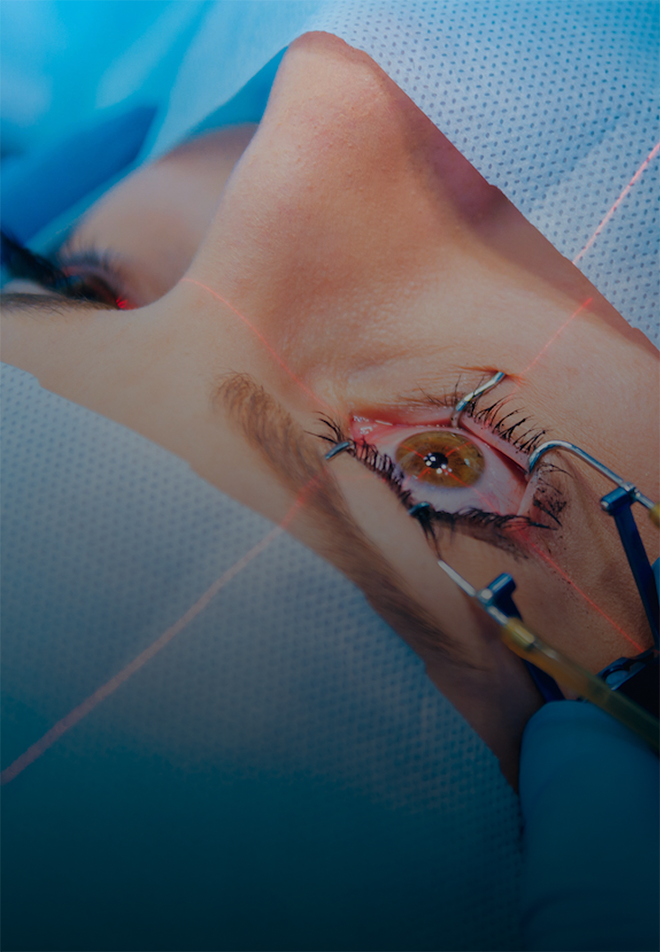
El trasplante de córnea, también conocido como queratoplastia, es un procedimiento oftalmológico vital para restaurar la visión en pacientes con diversas afecciones corneales, como queratocono avanzado, cicatrices corneales, distrofias corneales o edema corneal grave. Antes de la cirugía, se lleva a cabo una evaluación exhaustiva del paciente para determinar la salud ocular general y la idoneidad para el trasplante. Los protocolos preoperatorios incluyen pruebas de la visión, topografía corneal, paquimetría y análisis de la salud ocular en general.Durante la cirugía de trasplante de córnea, se extrae la córnea dañada y se reemplaza con tejido corneal donado, conocido como injerto. Dependiendo de la técnica utilizada, el injerto puede ser de espesor completo (queratoplastia penetrante) o de espesor parcial (queratoplastia lamelar). La cirugía se realiza generalmente bajo anestesia local y puede durar varias horas, dependiendo de la complejidad del caso.Los protocolos postoperatorios son cruciales para garantizar una recuperación exitosa y prevenir complicaciones. Esto incluye el uso de medicamentos para prevenir la infección, controlar la inflamación y promover la cicatrización, así como el seguimiento regular con el oftalmólogo para monitorear la salud ocular y ajustar el tratamiento según sea necesario. Los pacientes deben seguir estrictamente las instrucciones postoperatorias, incluido el cuidado de los ojos y la protección contra lesiones.Es importante destacar que el trasplante de córnea es un procedimiento altamente especializado que requiere la colaboración entre el paciente, el oftalmólogo y el banco de tejidos para garantizar la seguridad y la eficacia del procedimiento. Aunque el trasplante de córnea puede mejorar significativamente la visión y la calidad de vida del paciente, también conlleva riesgos y posibles complicaciones que deben ser discutidos con el médico.En resumen, el trasplante de córnea es una intervención oftalmológica crucial para restaurar la visión en pacientes con afecciones corneales graves, y sigue protocolos específicos para garantizar resultados óptimos y una recuperación exitosa.